The new expert sub-committee report on which the latest ban on fixed dose combination drugs or FDCs is based is far more rigorous than the earlier report in 2016. It justifies a complete prohibition of the drugs – not merely restriction or regulation – by noting that public health is integral to public interest. This report provides also provides the first steps for revamping the architecture of India’s dysfunctional system of drug regulation.
On September 12, the Ministry of Health and Family Welfare issued a fresh set of notifications banning 328 FDCs. This was a replay of its action in March 2016, when 344 FDCs were prohibited in the public interest under section 26A of the Drugs and Cosmetics Act, 1940. Since then, the ministry has had to fight off an onslaught of legal challenges by deep-pocketed pharmaceutical companies.
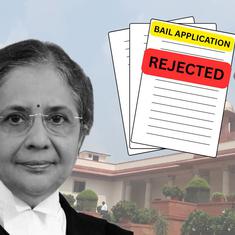
The Delhi High Court overturned the 2016 ban on an incorrect interpretation of the Drugs and Cosmetics Act that the government should have first consulted the Drugs Technical Advisory Board or DTAB. Although the Supreme Court disagreed with the High Court interpretation, the apex court’s December order left the government back at square one. The Supreme Court concluded that the Kokate Committee report on which the government had relied was not well-reasoned and ordered the DTAB or its sub-committee to re-examine the drugs that had been banned.
Although they are already making attempts, pharmaceutical companies will have a hard time poking holes in the report of the new sub-committee headed by Dr Nilima Kshirsagar, chair of clinical pharmacology with the Indian Council of Medical Research. Where the Kokate committee report relied on a few stock articles, the new report is more rigorous in referring to Cochrane reviews and standard treatment guidelines and in consulting websites of drug regulatory authorities in other jurisdictions.
The report also explicitly links the evidence on FDCs to the three criteria for prohibiting the manufacture of a drug in section 26A – that the FDCs poses a risk to human beings or animals, that they do not have the therapeutic value claimed or that they contained such ingredients and in such quantities that there is no therapeutic justification for them.The report notes that any one of these criteria is injurious to public health, thereby making it necessary and expedient to prohibit the drugs in the public interest. The public interest also has an economic dimension, with the report noting that FDCs with no therapeutic justification are “an unnecessary and unjust burden on the pockets of poor people”.
Evidence of systemic failure
While the report serves the purpose for which it was commissioned in rebutting the arguments of pharmaceutical companies, it indirectly provides a roadmap for the overhaul of India’s drug regulator. The report points to three main areas to be addressed – pharmacovigilance, technical capacity for drug approval, and lapses in the approval process especially at the state level.
Companies argued that the lack of reports about adverse drug reactions should be proof of their safety. The report brushes this aside by pointing to the absence of an active pharmacovigilance system in India. (The absence of a robust materiovigilance programme was also noted by the expert committee report on the Johnson & Johnson hip implants.)
Companies also argued that the Drugs Controller General India had approved FDCs with “similar” components to those being considered by the sub-committee. The sub-committee has responded by stating that it has taken into account factors that the DCGI might not have considered. While the function of approving drugs is different from prohibiting them in the public interest, it is hoped that the DCGI will apply the same standards to judge the evidence submitted by pharmaceutical companies as regards the safety and efficacy of the drug, in particular, as regards the quality of clinical trials conducted.
The DTAB appears to have recognised the need to build technical capacity in approval processes. At its 80th meeting, it recommended that guidance and training material on FDCs be prepared for both applicants and stakeholders, which would include various subject expert committees that review applications for the approval of new drugs.
The sub-committee also notes that companies were not able to furnish proof of the indications for which the FDCs were approved, a glaring failure of the regulatory system and especially of State Licensing Authorities that issued these approval letters. There simply cannot be any marketing approval for a drug independent of the use for which it is intended. The report cites several examples of FDCs for which the package insert was not submitted. The package insert provides information to prescribers and patients on the use, contra-indications and side-effects of the drug and must be submitted to the DCGI at the time of approval. The fact that companies with drugs on the market were unable to provide copies of these inserts is worrying.
Legal battle continues
The Central Drugs Standards Control Organisation should be applying its mind to these systemic problems. Instead, it is firefighting in the Supreme Court as pharmaceutical companies pose challenges to the fresh ban. A critical bone of contention appears to be 15 FDCs that received approval before September 21, 1988 – that is, before rules for the FDC approval were introduced. The Supreme Court set aside the notifications banning these FDCs on the grounds that they should not have been referred to the Kokate Committee at all. The Kokate Committee’s remit was to examine FDCs that had not received due approval from the DCGI; companies have argued that this Central approval was not required before 1988. However, the court left it open to the central government to start over and carry out an inquiry into whether these drugs could be banned under section 26A.

The sub-committee has examined these 15 FDCs. It draws the basis for this from the DTAB’s decision to ask the sub-committee to submit a report on these 15 FDCs as well. However, in an order dated September 7, the Supreme Court prohibited the central government from acting on the sub-committee’s report as regards these 15 FDCs. On September 17, companies selling drugs like Saridon, Piriton and Dart claiming pre-1988 approval, approached the court to be allowed to continue their manufacture and sale. The Court has permitted this subject to the final outcome of the proceedings.
There are two main problems with this – first, it is unclear what procedure the Supreme Court had in mind when it said that the central government could carry out a fresh inquiry into the pre-1988 drugs. The sub-committee has conducted a fresh inquiry into these drugs. The DTAB was perfectly within its rights to entrust this task to the sub-committee. It surely cannot be the court’s reasoning that 328 drugs ought to be considered by one committee and 15 drugs by another. This would be an absurd waste of time and regulatory resources.
Second, while the court continues to permit companies to sell their drugs pending a final decision, its orders do not make note of the potential harm to public interest against the alleged financial harm to the companies. The sub-committee has stated that several companies that claimed pre-1998 approval could not furnish documentary proof of approval. Given that something as vital as public health is at stake, and cognisant of its own lengthy proceedings, the court must hear arguments to decide in whose favour the stay should lie. If not, there is danger of clever lawyering undoing this small, but vital step towards reforming India’s drug regulation and protecting public health.
The writer is senior resident fellow at the Vidhi Centre for Legal Policy, New Delhi.