On May 17, the government medical college of Jammu, the main tertiary care hospital in the district, received a terse letter from the health department underlining the need for “corrective measures” to reduce deaths among Covid-19 patients.
“It is desirable that the senior faculty members of the concerned departments of your institution be directed to increase their presence by making frequent rounds of wards, where the COVID positive patients are admitted, so that such patients are properly looked after and treated, which will help us in reducing the mortality also,” stated the letter issued by Atal Dulloo, financial commissioner in the health and medical education department.
In the second-wave of Covid-19 in Jammu and Kashmir, the administration is facing a peculiar challenge: high mortality among Covid-19 patients in the Jammu division.
Since the start of the pandemic in March 2020 until March 31 this year, the mortality rate in Jammu was lower at 1.38% compared to 1.60% in Kashmir. But with the onset of second-wave in April, Jammu has been witnessing overwhelmingly more deaths despite having fewer cases than Kashmir.
From April 1 till May 17, Jammu and Kashmir recorded a total number of 1,16,531 Covid-19 cases, with Kashmir accounting for more than 73,000 cases and Jammu for 43,000 cases. Yet, Jammu saw 756 deaths, compared to 468 deaths in the Valley.
As a result, the mortality rate in Jammu has jumped up to 1.80%, higher than the national mortality rate of 1.11%.
The higher mortality rate in Jammu has alarmed the government which has tasked healthcare experts and doctors to assess the reasons for it. On May 15, the government medical college, Jammu, announced that the B.1.617 variant of the virus was responsible for the recent surge in Covid-19 cases in the region. Classified as a “variant of concern” by the World Health Organisation, the B.1.617 variant, first detected in India in October, now found in at least 44 countries, is more infectious, say scientists.
In March, genome sequencing of Covid-19 samples from Jammu had found a variant first detected in the United Kingdom in more than 60% samples. “However, in April the %age of UK Variant dropped to 47% and B.1.617 increased from 5.8% to 38%,” the statement by the government medical college, Jammu, noted.
But healthcare experts say the higher mortality rate in Jammu cannot be directly put down to the presence of the B.1.617 variant. Instead, they link the fatalities with the structural deficiencies in the region’s healthcare sector, which is plagued by a shortage of health workers, as well as the absence of a vibrant non-governmental sector unlike Kashmir.
Chronic healthcare gaps
Jammu and Kashmir government’s advisory committee on Covid-19 management has submitted two reports on the situation in Jammu region so far. Constituted in June last year to advise the government on fighting the pandemic, the committee has 10 senior specialist government doctors and experts as members. Two members spoke to Scroll.in on the condition of anonymity.
“Variants of the virus had likely got introduced in Jammu very early on because of Jammu’s proximity and ease of access with Punjab, Haryana and Delhi where the Indian variant has been traced as well,” said one of the members, a senior doctor.
The prevalence of the highly infectious variant quickly overwhelmed the healthcare system, the official data shows. Since the onset of pandemic in March last year, Jammu region recorded 52,941 Covid-19 cases till March 31 this year. The region saw 736 Covid-19 deaths in the span of a year. However, since April 1, the region recorded more than 46,000 cases and 835 deaths in less than two months. Jammu’s healthcare system was ill-equipped to deal with the surge.
According to the senior doctor, Jammu region lacks robust healthcare infrastructure compared to Kashmir. “The distances between the urban tertiary care hospitals in Jammu and the peripheries are large, which is not the case with Kashmir,” he said. “The infrastructure at the peripheries is not good. So, the patient might not get proper medical care on time.”
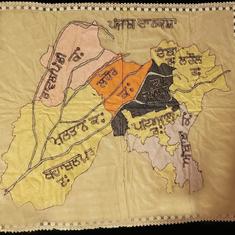
The union territory of Jammu and Kashmir comprises 20 districts, ten each in Kashmir Valley and Jammu region. Kashmir accounted for 55% of the population of the erstwhile state, according to the 2011 census. While remote areas in Kashmir are relatively well-connected with district centres and healthcare institutions in Srinagar city, the same doesn’t hold true for far flung areas of the Jammu region.
In January 2018, a Right to Information application revealed that out of 259 health centres located in remote hilly areas of the Jammu division, doctors were posted only in 75 of them.
The crisis is aggravated by the centralisation of tertiary care infrastructure in and around the city of Jammu. “In Kashmir, we see that a lot of burden is being shared by district level hospitals and zonal Medical Colleges,” said a consultant doctor, who is a member of the advisory panel. “That reduces a lot of burden on healthcare in Srinagar city.”
Another factor that contributed to the crisis in Jammu division, said members of the advisory panel, was the thrust on private practice by the government doctors. “Somewhere we feel a doctor’s commitment to hospital practice is not as developed as you have in Kashmir,” said the senior doctor. “They are involved in a lot of private practice, which is also a service, but at this moment, the focus should be on dedicating resources and time on hospital practice.”
The May 17 order, asking senior doctors to supervise the treatment of Covid patients in Jammu, is part of the many suggestions forwarded to the government by the committee. “We are glad that the government has appreciated it now but we have been aware of this problem since long,” the senior doctor added.

Lack of manpower
Social activist Balvinder Singh knows the healthcare infrastructure of Jammu region like the back of his hand. For years, he has been relentlessly exposing the loopholes in the sector and trying to nudge the government in action through petitions before the Jammu and Kashmir High court.
In April, a Right to Information application by Singh had revealed a shortage of personnel at the government medical college, Jammu, and its associated five hospitals. The college and hospitals form the core of the medical care infrastructure in Jammu for Covid-19 patients. “There was 30% shortage of faculty members and 70% shortage of super specialists at these hospitals,” Singh said. “And these are the figures of February this year.”
The lack of manpower isn’t restricted to doctors alone: 136 posts of nursing staff, 73 posts of paramedics and 147 posts of Class IV employees were lying vacant, Singh’s application revealed. “Ideally, we should have more than adequate human resources available but that is unfortunately not the case,” Singh said.
The government seems to have finally woken up to the gaps. On May 16, Dr Shashi Sudhan Sharma, principal and dean of the government medical college, Jammu, informed Lieutenant Governor Manoj Sinha that as many as 250 nurses would join the hospitals within three days. The same day, Union Minister Dr Jitendra Singh, who represents Udhampur constituency of Jammu in Lok Sabha, said the government was deploying medical and nursing students for ward duty at the hospital.
Delayed hospitalisation
Not only does Jammu have chronic healthcare deficits, it also has poor public awareness on Covid-19, said the consultant who is a member of the advisory panel. “In many cases, we have seen patients only rushing to the hospital when the patient’s condition has already worsened,” he said.
The consultant’s assessment is seconded by the Jammu and Kashmir government’s own findings about Covid-19 mortalities in the union territory. Out of 806 deaths which occurred in the union territory between April 15 and May 12, nearly half were of those who died within three days of their hospitalisation, “thus indicating that they were well into late stages of infection before they got tested”, a study by the Jammu and Kashmir wing of the National Health Mission revealed.
This assessment, according to the consultant, made them stress upon the government the need to increase public awareness about the deadly virus. “We suggested they go with loudspeakers in each and every village and make people aware,” he said.
Absence of NGOs
The crisis has also highlighted a vacuum in the non-government sector in Jammu. “There are some small groups helping with oxygen supplies and cremations but not on a big scale like Kashmir Valley,” said the activist, Balvinder Singh. “I must salute the volunteer groups in Kashmir for what they are doing.” He was critical of civil society groups within the Jammu region, who according to him, has failed to make their presence felt on the ground.
As compared to Jammu, Kashmir valley has a robust and an experienced network of charity groups and non-government organisations that are helping out patients with oxygen supply, concentrators, transportation, medicines and even burials. “Kashmiri society is battle-hardened due to the situation in the last three decades here, so we know how to handle a crisis,” said a doctor at one of Srinagar’s premier tertiary care hospitals.
He offered an example to make his point. “Ideally, a patient who needs oxygen has to be admitted in the hospital but what we are doing is that they are being provided oxygen and other support inside their homes by these volunteer groups while we offer consultancy to them on phone,” he explained. “Something like that in Jammu would have really helped ease the burden on hospitals there.”